For full functionality of this site it is necessary to enable JavaScript. Here are the instructions how to enable JavaScript in your web browser.
Welcome to the NOGG 2024 Guideline. These new thresholds ensure equality of access to treatment for older patients with and without fracture, and identify a group who are at very high fracture risk who should be considered for specialist referral (for full details, see the Full Clinical Guideline).
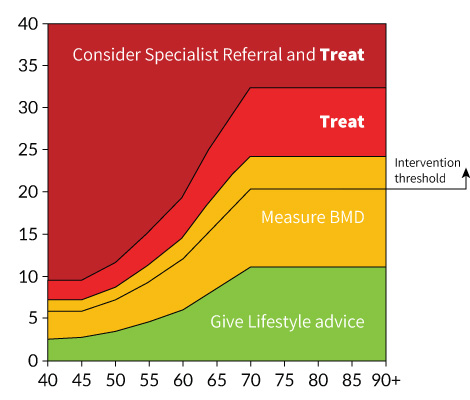
Intervention Thresholds
(%) 10-year probability of
Major Osteoporotic Fracture

Age (years)
Interpretation
Following the assessment of fracture risk using FRAX® in the absence of BMD, the patient may be classified to be at low, intermediate, high or very high risk.
Where both the MOF and Hip fracture probabilities fall below the treatment threshold, lifestyle advice should be given and a further assessment is recommended in 5 years or less depending on the clinical context (e.g. new clinical risk factors develop, or a fragility fracture occurs).
- Low riskgive lifestyle advice, and reassess in 5 years or less depending on the clinical context.
- Intermediate riskmeasure BMD and recalculate fracture risk. If BMD measurement not practical (e.g. , frailty) or is unavailable, offer treatment if risk is at or above the Intervention Threshold shown.
- High riskoffer treatment to reduce fracture risk.Measure BMD to guide drug choice and provide a baseline for BMD monitoring.
- Very high risk Consider referral to osteoporosis specialist for assessment and consideration of parenteral treatment. If a delay anticipated, start oral treatment in meantime. If not for referral, treat as for high risk.
NB - These thresholds are for guidance only and the final decision to assess BMD or to initiate therapeutic intervention lies with the individual clinician.
'Consider' indicates a conditional recommendation, which applies when the clinician examines the evidence within the wider health and social context and discusses the choices with the patient, taking into account the patient’s values and preferences, or where documentation of the discussion of the pros and cons of an intervention is the indicator of quality, rather than the course of action itself.
Management
- For a more detailed description of investigations and treatments, please refer to the Full Guideline.
- Arithmetic adjustments can be applied to FRAX probabilities of hip fracture and major osteoporotic fracture to take into account some common clinical scenarios.
- Consider the level of fracture risk, any additional clinical risk factors, patient choice, and the cost-effectiveness of treatment, when deciding on a particular drug treatment.
- Assess falls risk in patients with osteoporosis and/or fragility fractures and offer those at risk an exercise programme to improve balance and muscle strength.
Treatment options in postmenopausal women, and men age ≥50
High risk
- Offer oral bisphosphonates (alendronate or risedronate) or intravenous zoledronate. Alternative first line options include denosumab, ibandronate, hormone replacement therapy, and raloxifene.
- Offer intravenous zoledronate as a first-line treatment option following a hip fracture.
Very high risk
- Consider anabolic (bone-forming) drug treatments as first-line treatment in those at very high fracture risk, particularly in those with vertebral fractures.
General advice
- Offer calcium and/or vitamin D supplementation if needed.
- Treat vitamin D deficiency and insufficiency prior to initiation of parenteral anti-osteoporosis drug treatment.
- Reassess fracture risk and start treatment promptly following a fragility fracture.
Treatment options in glucocorticoid-induced osteoporosis
High risk
- Offer oral bisphosphonates (alendronate or risedronate) or intravenous zoledronate as first-line drug options. Denosumab is an alternative option.
- Offer intravenous zoledronate as a first-line treatment option following a hip fracture.
Very high risk
- Consider Teriparatide as a first-line drug option in those at very high fracture risk.
General advice
- Offer calcium and/or vitamin D supplementation if needed.
- Treat vitamin D deficiency and insufficiency prior to initiation of parenteral anti-osteoporosis drug treatment.
- Reassess fracture risk and start treatment promptly following a fragility fracture.
- Start bone-protective treatment at the beginning of glucocorticoid therapy in the following (bone density assessment should follow later):
- anyone with a prior fragility fracture,
- women age ≥70 years,
- postmenopausal women, and men age ≥50 years, prescribed high doses of glucocorticoids, i.e., ≥7.5 mg/day of prednisolone
- postmenopausal women, and men age ≥50 years, with a FRAX probability of major osteoporotic fracture or of hip fracture exceeding the intervention threshold.
- Bone protective therapy may be appropriate in some premenopausal women and younger men. Caution is advised whenprescribing drug treatment in women of childbearing age. Referral of complex cases to secondary care is often necessary.