Information for patients and the public
Updated December 2024
Download the information leaflet as a PDF file
Introduction
This information is written for patients and the public. It explains the Clinical Guideline written by the UK National Osteoporosis Guideline Group (NOGG). Healthcare professionals use this Guideline to manage people’s osteoporosis.
Osteoporosis is a condition in which bones have become weaker. This means they are more likely to break when we have no injury, or a minor bump, or fall from standing height or less. A break like this is called a fragility fracture.
As we get older, from around the age of 40 onwards, our bones gradually get weaker. This is part of the natural ageing process. For both women and men there is a steady decline in bone strength. In women there is a bigger drop after the menopause due to hormonal changes. There are also other medical conditions and treatments that may affect our bones. This loss in bone strength is a combination of the density (quantity) and the structure (quality) of our bones. It varies from one person to another for many reasons.
The World Health Organization (WHO) defines osteoporosis using a T-score, which is a measure of bone density compared to average healthy women in their 20s. T-scores apply to men and women. Osteoporosis is defined as a T-score of -2.5 or less.
The effects of osteoporosis vary considerably. Some people have no fractures and therefore no symptoms at all. Some people have fractures and recover fully. Others may have more long-lasting effects from fractures, such as difficulty walking, or pain, or needing help with daily activities.
Healthcare professionals such as your GP, or a nurse, doctor or consultant at a clinic or hospital may ask you about risk factors for osteoporosis. These are things in your life that could mean you are more likely to have weaker bones, which increases your chance of having a fragility fracture. They use this information with the Guideline to help them decide on the treatment options for you to reduce the chance, or risk, of having a fragility fracture. There is also guidance on how to help you if you have had painful or disabling fractures, especially in the spine.
The Guideline contains a lot of technical detail about identifying who is at risk of a fracture, how risk is best assessed, lifestyle approaches including exercise and diet, and which drugs to use and when. The most important points are:
Who Is At Risk Of Fracture?
The Guideline main covers postmenopausal women, and men over 50. In this group, 1 in 2 women and 1 in 5 men are currently expected to have a fragility fracture in their lifetime. This includes spinal fractures, as well as hip, wrist, and other bones. Anyone in this group who has a fragility fracture, or may be at risk of having a fragility fracture, should be assessed.
You don’t have to break a bone before your risk of fracture can be assessed.
Osteoporosis in younger people and in pregnancy is rare and needs specialist care.
What Does Fracture Risk Assessment Mean?
The preferred method for assessing fracture risk uses an internet-based system called FRAX. This is an anonymous questionnaire about risk factors that uses a computer programme to calculate your risk of fracture over the next 10 years. For example, a risk of 20% means that out of 100 people like you, 20 will fracture a bone some time over the next 10 years.
FRAX can be used by a healthcare professional to assess the chance of any postmenopausal woman, or man over 50, breaking a bone. The questionnaire asks about age, previous fractures, parents’ fractures, body weight and height, smoking, alcohol consumption, rheumatoid arthritis, use of steroid tablets, and other related conditions or treatments.
According to your level of risk you may need to have a bone density scan called DXA. This scan helps to judge your fracture risk more accurately, by measuring bone density in your hip and spine.
Vertebral fracture assessment (VFA) is another type of DXA scan. It looks for fractures in the spine. It is performed if your bone density is low, or you have lost height (usually more than 4cm), or you have certain other medical conditions with acute back pain.
How Is Treatment Decided?
First your healthcare professional looks at your health record and asks you some questions to check your level of risk. Then FRAX indicates whether drug treatment is needed depending on the level of risk, your risk factors, and your own preferences. Either way, you should receive advice about what lifestyle measures you can take to help your bones.
Postmenopausal women, and men over 50, who have had a recent fragility fracture are usually offered a drug treatment. A risk assessment, and sometimes a DXA scan, should be advised before making a treatment choice.
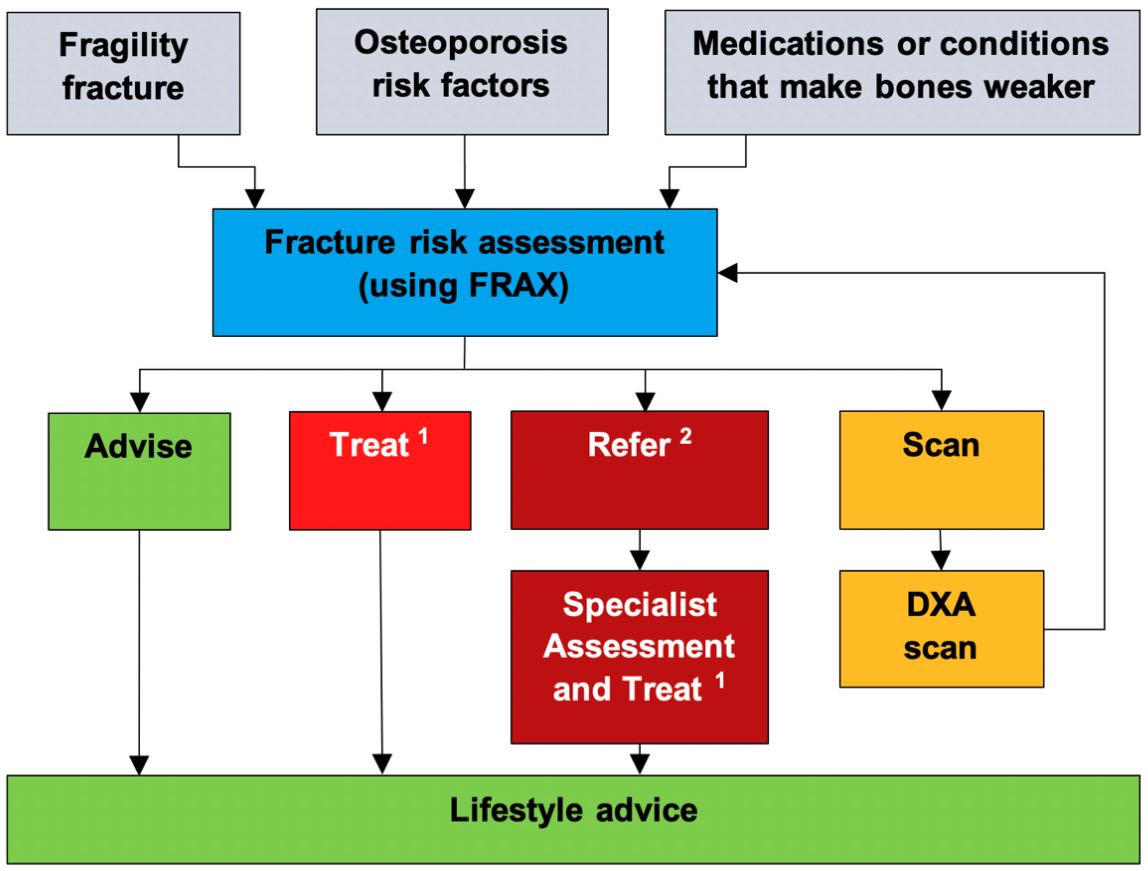
1 Treat means investigation and treatment. Investigation is sometimes necessary, such as a
blood test. Treatment means a bone strengthening drug.
2 Refer means that a Specialist should assess you and discuss your treatment options with
you.
What Drug Treatments Are Recommended?
The main treatments for men and women are alendronate or risedronate tablets taken once a week. There are other drugs available if these are not suitable, or if your risk is higher and you need an alternative treatment. In this case you may be referred to a specialist.
What Lifestyle Changes Are Recommended?
Lifestyle advice for everyone includes a healthy, well balanced diet with the right daily intake of calcium and vitamin D, regular weight-bearing and muscle strengthening exercise, advice not to smoke and limit alcohol intake, and measures to reduce your risk of falling over.
What Should I Expect?
Your healthcare professional will explain your risk level and what that means for you, and will discuss the best course of action.
If you have already had a fragility fracture, you should have access to a Fracture Liaison Service that can assess you.
Osteoporosis treatment takes years, as it takes time for the drugs to work. You should have a review in the first year to check that you are happy taking the medication, and a re-assessment of your risk at least every 5 years. Most osteoporosis tablets are recommended for at least 5 years, or 10 years if you are over 70 or have broken bones in the past.
If your treatment is stopped, you should have a new assessment of your fracture risk within 3 years, or straight away if you have a new fracture.
NOTE: in Scotland there is an osteoporosis guideline provided by SIGN (Scottish Intercollegiate Guidelines Network) which has slightly different advice about assessment and treatment.
These important actions can reduce some of the risk factors listed earlier:
- a healthy diet, with supplements of calcium and vitamin D if necessary
- stopping smoking and not drinking excessive amounts of alcohol
- taking regular exercise that is suitable for you
- if you are taking medication for osteoporosis, do follow the instructions and take it regularly
- if the medication is causing you problems, do tell your doctor or clinician because there are good alternatives (besides just taking calcium and vitamin D)
It can help if you know something about the condition, and if you talk to others about it. One way to do this is to join a relevant charity and get involved in supporting it. See Further Information below.
The National Osteoporosis Guideline Group (NOGG) was formed in 2007 by a group of osteoporosis experts. In addition to the 19 specialists who advised on and wrote the Guideline, the following organisations are supporting it:
The Association for Clinical Biochemistry and Laboratory Medicine, Bone Research Society, British Geriatrics Society, British Orthopaedic Association, British Orthopaedic Research Society, British Menopause Society, British Society for Rheumatology, European Calcified Tissue Society, European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases, International Osteoporosis Foundation, Osteoporosis Dorset, Osteoporosis 2000, Primary Care Rheumatology and Musculoskeletal Medicine Society, Royal College of Physicians, Royal Osteoporosis Society, Royal Pharmaceutical Society, Society for Endocrinology, and The Nutrition Society.
The national charity specialising in osteoporosis, with comprehensive information and support is:
- The Royal Osteoporosis Society www.theros.org.uk 0808 800 0035
Two regional charities also providing osteoporosis support to patients are:
- Osteoporosis 2000 (Sheffield) www.osteoporosis2000.co.uk 0114 234 4433
- Osteoporosis Dorset www.osteodorset.org.uk 01202 443064
NOGG online includes links to all supporting organisations:
Links for other information:
Local Support Groups where you can connect to people in your area:
A balanced diet, calcium-rich foods, and a calcium calculator:
Stopping smoking and reducing alcohol:
Suitable exercises: